Fax (215) 947-7501
Mohs Surgery
What is Mohs Surgery?
Before Surgery
The Day of Surgery
After Surgery
Frequently Asked Questions
What is Mohs Surgery?
Mohs Surgery is the most effective treatment for many types of skin cancer. The goal of Mohs surgery is to remove as much of the skin cancer as possible, while doing minimal damage to surrounding healthy tissue. It is an outpatient procedure, performed under local anesthesia, and is distinguished by a specific technique of tissue examination that is unique to Mohs surgery. The term “Mohs” refers to Dr. Frederic Mohs, Professor of Surgery at the University of Wisconsin, who developed this surgical technique in the 1930s. Dr. Mohs recognized that a skin cancer often resembles the “tip of the iceberg” with more tumor cells growing downward and outward into the skin like the roots of a tree. These “roots” are not visible with the naked eye, but can be seen under a microscope. The Mohs surgical process involves a repeated series of excisions, followed by immediate microscopic examination of the tissue to assess if any tumor cells remain. The pathological interpretation of the tissue margins is done on site by Dr. Regan, who is specially trained in the reading of these slides and is best able to correlate any microscopic findings with your surgical site. The result is a surgical procedure that offers outstanding cure rates while also minimizing the cosmetic impact of the treatment.
What are the Advantages of Mohs Surgery?
- Ensuring complete cancer removal during surgery, virtually eliminating the chance of the cancer growing back
- Minimizing the amount of healthy tissue lost
- Maximizing the functional and cosmetic outcome resulting from surgery
- Repairing the site of the cancer the same day the cancer is removed, in most cases
- Curing skin cancer when other methods have failed
Why does my skin cancer need Mohs surgery?
Mohs surgery is used for skin cancers which are at higher risk for forming subclinical extensions or “roots” which are invisible to the eye. These cancers can be much bigger than they look on the surface, much like the tip of an iceberg. Mohs surgery is indicated in the treatment of skin cancers:
Before Surgery
Pre-operative consultation
Prior to scheduling your procedure, you will first have a detailed Mohs pre-operative consultation. This consultation is important to examine your skin cancer, evaluate your medical history, explain the procedure in detail, and to make sure we do not need to do any further testing or referrals prior to the surgery. Because all skin cancers are not alike, the course of treatment is determined by the type of skin cancer. The pre-operative consultation will allow us to determine if Mohs surgery is the best treatment for you.
How to prepare for Mohs surgery
Other things you should do or know prior to your Mohs surgery include:
Medications
Take all of your usual medications including insulin on the day of surgery unless directed otherwise.
If you are taking aspirin, ibuprofen or other non-steroidal anti-inflammatory medication for headaches, pain or as a preventive measure, stop taking these medications for at least two weeks (aspirin) or two days (ibuprofen and others) before surgery and for three days after surgery. These products may increase bleeding during or after surgery.
Things to Avoid
Stop tobacco use for as long as possible before and after surgery to permit the best possible healing. Using tobacco can slow or impair proper healing
Avoid alcohol for 48 hours before and 48 hours after the surgery; alcohol causes excessive bleeding.
The night before surgery
You may want to wash your hair the night or morning before surgery because you will be asked not to shower for 24-48 hours after the surgery. Do your best to get a good night’s rest prior to the surgery. Unless instructed otherwise, you are free to eat and drink as usual. Bring a book, computer, or other activities to keep you busy while you are waiting, because you may spend the better part of the day at our office. If you have a history of high blood pressure or anxiety, you may wish to avoid caffeine on the day of your appointment. Your surgery will need to be rescheduled if your blood pressure is too high.
Please do not apply creams, make-up, or after shave lotions near the surgery site on the day of your procedure. Please do not wear jewelry on the day of your procedure.
Be prepared to be at the office for the entire day.
The Day of Surgery
When you arrive at the office, you will check in at the front desk and have a seat in the waiting room. A surgical assistant will then bring you back to one of our surgical rooms.
Step 1: Anesthesia
The tumor site is locally infused with anesthesia to completely numb the tissue. General anesthesia is not required for Mohs micrographic surgery.
Step 2: Removal of visible tumor (Stage 1)
The first thin, saucer shaped “layer” of tissue is surgically removed by Dr. Regan. An electric cautery tip may be used to stop the bleeding.
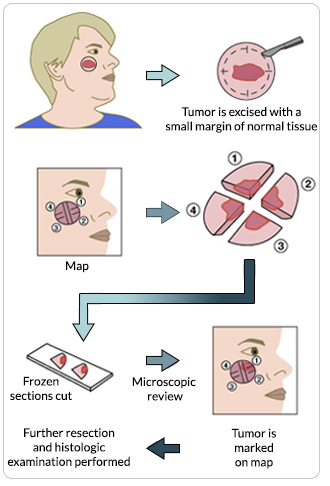
Step 3: Mapping the tumor
Once a “layer” of tissue has been removed, a “map” or drawing of the tissue and its orientation to local landmarks (e.g. nose, cheek, etc) is made to serve as a guide to the precise location of the tumor. The tissue is labeled and color-coded to correlate with its position on the map. The tissue sections are processed and then examined by the surgeon to thoroughly evaluate for evidence of remaining cancer cells. It takes approximately 60 minutes to process, stain and examine a tissue section. During this processing period, your wound will be bandaged and you may leave the operative suite.
Step 4: Additional stages – Ensuring all cancer cells are removed
If any section of the tissue demonstrates cancer cells at the margin, the surgeon returns to that specific area of the tumor, as indicated by the map, and removes another thin layer of tissue only from the precise area where cancer cells were detected. The newly excised tissue is again mapped, color-coded, processed and examined for additional cancer cells. If microscopic analysis still shows evidence of disease, the process continues layer-by layer until the cancer is completely removed. This selective removal of tumor allows for preservation of much of the surrounding normal tissue. Because this systematic microscopic search reveals the roots of the skin cancer, Mohs surgery offers the highest chance for complete removal of the cancer while sparing the normal tissue. Cure rates typically exceed 99% for new cancers, and 95% for recurrent cancers.
Step 5: Reconstruction
Fellowship-trained Mohs surgeons are experts in the reconstruction of skin defects. Reconstruction is individualized to preserve normal function and maximize aesthetic outcome. The best method of repairing the wound following surgery is determined only after the cancer is completely removed, as the final defect cannot be predicted prior to surgery. Stitches may be used to close the wound side-to-side, or a skin graft or a flap may be designed. Sometimes, a wound may be allowed to heal naturally.
After Surgery
What to expect after the surgery
Following your surgery, we will discuss postoperative care with you and you will be given written instructions on how to care for your wound.
Do not smoke – Smoking deprives your skin of oxygen, which is needed for healing.
Minor Post-Surgical Discomfort Expected
Bruising: Swelling and slight bruising are common following Mohs surgery. A “black eye” is common with surgery around the eye and on the forehead. These symptoms usually subside within 5 to 7 days after surgery and may be reduced by sleeping with your head slightly elevated and using an ice pack for short periods of time during the first 24 hours.
Pain: People are often surprised by how little discomfort they have after Mohs surgery. If you do have discomfort, it can usually be managed by Tylenol.
Options for Post-Surgical Reconstruction
Wound Healing, Scarring, and Scar Revision
In general, your postoperative scar will improve with time, taking 1 year or greater to fully mature. You will notice that for the first 1-2 months the scar will contract and become firm and lumpy. This is normal. On the face, this firmness will improve and soften significantly over time. The scar will also become red with an increased number of small blood vessels; this too will improve with time. Please minimize sun exposure to the scar as this can lead to darkening of the scar as well as increased blood vessel formation and further redness. If you have any problems with healing after surgery, Dr. Regan will be available throughout the process to ensure you have the best possible outcome.
Follow-up
This depends on how your wound is repaired. If your wound is repaired in a way that requires stitches, you may be asked to return in about 7-14 days to remove your stitches. If your wound is allowed to heal on its own (also referred to as second intention healing), you may be asked to return at 4 weeks and 8 weeks for Dr. Regan to check on your healing. Regardless of the above, it is typically recommended that you follow-up for a routine skin exam with your general dermatologist within 3-6 months; sooner, for any spots of concern.
I found a suspicious skin lesion; do I need Mohs Surgery?
If you have any type of suspicious skin lesion you should seek evaluation by a dermatologist. If skin cancer is suspected, he or she may recommend and perform a biopsy. Mohs surgery may be recommended based on the type and location of the skin cancer, as well as other factors.
How may skin cancer be treated?
There are a variety of successful methods of treating most skin cancers in most people. These include scraping and burning, cutting out and sewing up, x-ray treatment, and cryosurgery (freezing). About nine out of ten cancers treated by these methods will be cured of their cancer. It is that one out of ten patients with recurrent tumors and unusual types of tumors that may need Mohs surgery. It is important to emphasize however, that no method at any time, including the Mohs technique, can promise 100% cure rates.
Is Mohs surgery the best treatment option for all skin cancers?
Not all skin cancers require Mohs surgery. The procedure is usually selected for tumors growing in high-risk areas of the face such as the nose, eyes, mouth, ears and surrounding tissue. It is also selected for all recurrent tumors (those reappearing after having been removed), all large tumors and all tumors which look aggressive under the microscope. Your doctor will advise you on the technique that is appropriate for your particular condition.
Why bother with Mohs surgery?
Mohs surgery cuts out the bare minimum of normal skin needed for a high cure rate (95%-99%). This is important in critical areas. Once a tumor has come back, conventional treatment (cutting out, scraping and burning, radiation) offers only a 50% cure rate. Mohs surgery is worth the bother in order to ensure that all of the cancer removed with the smallest possible hole.
Will Mohs surgery leave a scar?
All surgical procedures have the potential for some degree of visible scarring. The appearance of a post-Mohs surgical scar will depend on several factors, including size and location of the final defect, individual skin characteristics, and the reconstruction options available. You should keep in mind, however, that the tissue-sparing nature of the Mohs technique may result in a smaller, less noticeable scar than other skin cancer removal methods.
How large of a wound should I expect and how will it be repaired?
Since we cannot know ahead of time the extent of the tumor, it is difficult to discuss how the wound will be repaired until the surgery is completed.
How painful is the Mohs procedure?
The area to be treated will be numbed by injecting a local anesthetic. This is usually the only part of the procedure that may produce discomfort. We will use a number of techniques to minimize any pain, so the injection is usually well tolerated.
Will my cancer come back?
Approximately 1-3% of skin cancers may grow back after Mohs surgery. This can be higher for certain high risk cancers. We recommend that you closely monitor your surgical site for recurrence of the skin cancer, and follow closely with your referring physician.
Why is My Picture Taken?
We photograph most patients before and after their surgery. These photos are used by us if the insurance company questions us regarding your claim and may also be used for teaching. We also send a picture to your referring physician.
How often must I return for follow-up visits once my wound is healed?
After the stitches come out we usually like to see you two months later. A period of observation of at least 5 years is essential. This follow up can be done by your Dermatologist. There are several reasons why this is important. Should there be a recurrence of the skin cancer after Mohs surgery, it may be detected at once and treated. Experience has shown that if there is a recurrence it will usually be within the first year following surgery. Studies have shown that once you develop a skin cancer there is a high risk that you will develop others in the years to come. You should watch for an open sore which does not heal and bleeds easily. If you notice any suspicious areas, it is best to check with your referring physician to see if a biopsy is indicated.
What happens on the day of the procedure?
Appointments for surgery are usually scheduled early in the day. You will be escorted into the surgical suite. The cancer may be outlined with a marking pen, then a local anesthetic is injected to numb the skin. The next step is to remove a thin layer of skin around the cancer. This tissue is carefully removed. An electric needle may be used to stop the bleeding. The assistant will then bandage you. By the time you get to the waiting room the removed tissue is already in our laboratory being processed for microscopic examination.
The most difficult part is waiting for the results of the surgery. This usually takes about an hour, though it may take longer. If the microscopic examination reveals that your tissue still contains cancer, the surgical procedure is repeated and the tissue again examined. Only the tissue containing skin cancer is removed. Several trips in and out of the surgical suite may be required the day that you are here.